Proponer una traducción mejor Proponer una traducción mejor | ||
INFORMACIÓN EXCLUSIVA PARA: MEDICOS, PARAMEDICOS, ESTUDIANTES DE MEDICINA.PRINCIPALMENTE. LOS INTERESADOS EN LA INFORMACION AQUI PLASMADA(LES RECORDAMOS QUE ESTA ES UNA INFORMACION MUY ESPECIALIZADA)EXCLUSIVAMENTE PARA EL ANALISIS POR MEDICOS Y AFINES,CON FINES EDUCACIONALES,TOMADOS DE LA LITERATURA INTERNACIONAL. ARTICULOS EN INGLES Y EN ESPAÑOL.
Mostrando las entradas con la etiqueta testosterona. Mostrar todas las entradas
Mostrando las entradas con la etiqueta testosterona. Mostrar todas las entradas
miércoles, 2 de septiembre de 2009
jueves, 27 de agosto de 2009
El hombre maduro(aging)
rom Geriatrics & Aging
Sexuality in the Aging Couple, Part II: The Aging Male
Irwin W. Kuzmarov, MD, FRCSC; Jerald Bain, BScPhm, MD, MSc, FRCPC
Published: 07/30/2009
Abstract
Sexual desire and activity continue well into later life, and advanced age alone is not a deterrent to a happy and healthy sex life; however, clinicians should be aware that the normal sexual response of men and women may change with aging. When sexual dysfunction occurs, studies show that men and women tend to view sexual dysfunction differently. Part I (which appeared in the November-December 2008 issue of Geriatrics & Aging) addressed sexual function and dysfunction with age in females. Part II of this two-part article series addresses sexuality and sexual dysfunction in aging men. For the emotional well-being of their patients, it is crucial that family doctors be aware of sexuality in the aging couple, and be able to evaluate and manage problems that may arise.
Introduction: Sexual Function and Dysfunction in Men
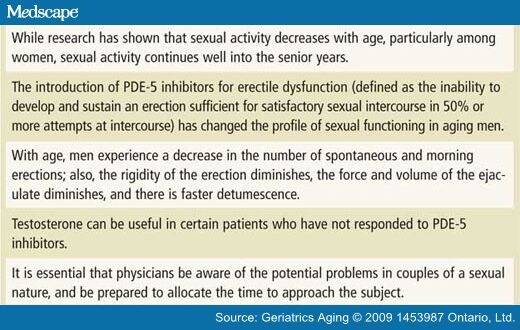
Evaluation of sexual responsiveness in older men and women has shown that sexuality and sexual activity continue well into later life, and that age-related changes do not necessarily prohibit sexual activity. While research has shown that sexual activity decreases with age, particularly among women, sexual activity in both men and women continues well into the senior years.[1-4] For example, Marsiglio et al., showed that 24% of people over age 75 were having sexual relations more than twice per month.[5]
Normal Sexual Response in Older Men
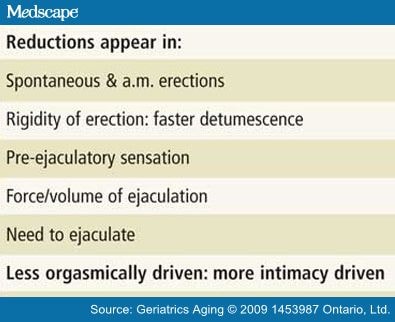
The normal male sexual response cycle is shown in Figure 1. There is a period of excitement followed by a plateau period, an orgasmic phase, a resolution, and a refractory period.[6] As men age, there are many changes that occur in their sexual response. This is shown in Table 1 .
Table 1. Sexual Function Changes with Age
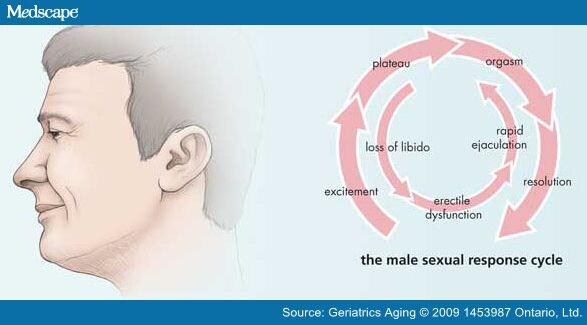
Figure 1. Sexual Response and Sexual Dysfunction in Males
In the previous article in this series, we discussed an emerging paradigm of women's sexual responsiveness that replaced a cycle of libido (desire)-arousal-orgasm-resolution with a model of intimate experience emphasizing that, while libido is maintained until quite late in the aging process, sexual arousal and response involve a sense of intimacy, bonding, commitment, love, affection, acceptance, etc., all of which may enter the sexual response equation, and result in pleasurable resolution, in which orgasm may or may not play a part. Similarly, with advancing age, some men may experience sexual response that is less orgasmically driven and more attached to a broader experience of intimacy.
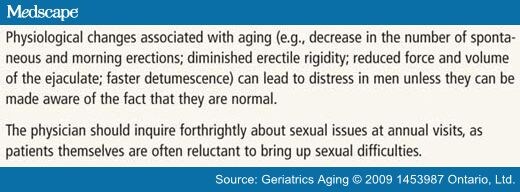
While sexual desire and response continue into late life, there are numerous physical alterations that can affect sexual activity. With age, men experience a decrease in the number of spontaneous and morning erections. The rigidity of the erection diminishes, the force and volume of the ejaculate diminishes, and there is faster detumescence. The preejaculatory sensation also diminishes. These changes often lead to distress in men unless they can be made aware of the fact that they are the normal changes of aging.
Many of these changes can be related to or exacerbated by several causes other than normal aging. These include lifestyle factors as well as cardiovascular, psychosocial, and psychiatric causes such as depression, all of which are prevalent in the aging population. These changes can lead to erectile problems and the development of erectile dysfunction. Antihypertensive drugs represent the single largest medication group implicated in the development of sexual side effects, including difficulties in attaining orgasm for both women and men.[7] Counselling of men as they age by their family physicians on the physiologic changes in their sexual performance, on the side effects that medications and other interventions may induce, and other intervening psychosocial factors may be helpful. This should be part of the annual visit, as well as part of the explanation given to men as medication or interventions are recommended and instituted.
Such counselling can start with simple information. Many men do not know what to expect as they age. Men may have less anxiety about the changes they are experiencing if they are made aware that they are normal and expected.
Sexual Dysfunction
Sexual dysfunction occurs when the normal pattern of sexual interaction between partners becomes interrupted and creates discontent in one or other of the partners or in the couple. In the female it is defined as any disorder related to sexual desire, arousal, orgasm, and/or sexual pain that results in significant personal distress and may impair the quality of life. Figure 2 shows the prevalence for male sexual dysfunction.[8] Loss of libido, erectile dysfunction, and rapid ejaculation are the three most significant and prevalent sexual complaints in this population.
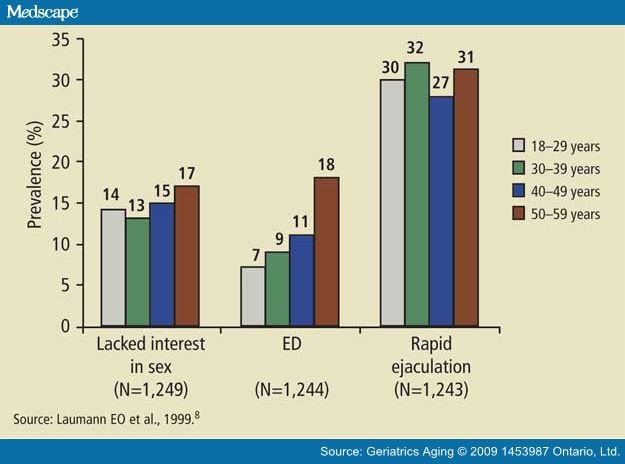
Figure 2. National Health and Social Life Survey: Prevalence of Male Sexual Dysfunction
Decrease in libido with age can be associated with various factors. These factors can relate to the psychosocial aspects of aging, which include the mental and physical status of both parties; the nature of their interpersonal relationship; marital conflicts and unresolved issues; and their overall lifestyles quality, including financial, social and, most important, communication issues.[9]
Other psychosocial stresses seen in older men that correlate with sexual dysfunction include the "Widower's Syndrome," which men may experience with the resumption of sexual activities after a period of celibacy. When a man has had the same sexual partner for many years, particularly a partner with whom he has enjoyed a satisfying marital life in general, and the partner dies, he may enter a new relationship with some trepidation. The trepidation may be amplified by erectile dysfunction, which he might not have experienced with his late wife. This may, of course, be due to newly manifested organic factors but it may also be due to the powerful impact of his psyche related to unconscious guilt that he is betraying the fidelity and happiness he enjoyed with his wife. These and other factors require more intense sexual and/or psychological counselling.
Note that alcohol consumption, poor physical fitness, diet, and lifestyle as well as concomitant comorbidities can also exert a negative pressure on libido. The loss of libido can also be related to low testosterone levels, which may be remediable through supplementation with exogenous testosterone.
Testosterone Therapies
Studies have shown that total testosterone does not correlate with levels of sexuality but that there are correlations between bioavailable testosterone and sexual desire and arousal, and erectile dysfunction occurs when the testosterone level falls below certain thresholds.[10-12]
It has been shown that testosterone levels decline with age; this progressive decline may begin as early as age 30.[13]Testosterone deficiency symptoms can include a loss of libido, fatigue, progressive decrease in muscle mass, erectile dysfunction, depression, and lack of concentration, as well as an increased risk of osteoporosis.[14] There is also evidence that testosterone can induce a response to phosphodiesterase type 5 inhibitors (PDE-5i's) in hypogonadal patients who have not responded to PDE-5 inhibitors prior to initiation of testosterone therapy. If there is evidence of hypogonadism, the addition of testosterone is indicated and may improve sexual interest. Recent evidence suggests that testosterone replacement among men with hypogonadism can provide significant sexual, physical, and psychological benefits.
Testosterone therapy is supplied in a variety of dosage forms, including oral, transdermal (gel or patch), and intramuscular preparations. With appropriate pretreatment investigations and regular assessments of efficacy, safety and treatment adherence, testosterone therapy can safely be used to improve the well-being of aging men experiencing symptoms of testosterone deficiency. It should be noted that there is emerging evidence for no increased risk of prostate cancer in men treated with testosterone therapy.[15]
Erectile Dysfunction and PDE-5 Inhibitors
The incidence of erectile dysfunction (defined as the inability to develop and sustain an erection sufficient for satisfactory sexual intercourse in 50% or more attempts at intercourse) is well documented particularly in the Massachusetts Male Aging study, where greater than 50% of men had some degree of symptom.[12] The relationship with diseases such as diabetes mellitus, cardiovascular disease, hypertension, neurological disorders, and psychiatric conditions such as depression, as well as medication, has been well described.
The introduction of PDE-5i's for erectile dysfunction has changed the profile of sexual functioning in aging men. The increasing use of PDE-5i's, the emerging understanding of the role of testosterone decline in men as they age, and the availability and use of adjunctive testosterone therapies have played a role in restoring men's sexual potency and libido.
The use of PDE-5 inhibitors has proven very effective in alleviating the physical effects of reduced erectile function in many men. This has generally been a constructive addition to the management of sexual dysfunction and relationship issues concerned with sexuality. It has, however, created consternation in some female partners who have interpreted the use of these agents as a sign of diminished interest in sex in general or with them specifically. The addition of a foreign agent, namely a drug to produce an erection, has been perceived as a sign that the partner is no longer attractive and is not desirable. The misperception is that the drug is preventing rather than promoting a healthy sexual relationship. For the first time, women who have never required their partners to be artificially stimulated to become erect are placed in this situation. The lack of understanding about the erectile response of their partner, and the role that medication or other devices play fuels this negative response. There are many couples who face this catch-22 situation in which the male partner's libido remains at a level satisfactory to him but who for largely organic reasons has erectile dysfunction remediable by a PDE-5i. In such a circumstance it would be useful to invite your male patient to return with his partner for a brief discussion about the causes of erectile dysfunction. In only a small minority of instances is the male's loss of libidinous interest in his wife the major cause of his ED. If this is the case he is usually aroused to erection by other stimuli.
The family physician, the urologist, the sex therapist, or the psychologist who deals with erectile problems in couples must explain the role and function of the erectile aids. The provision of PDE-5i's to aging patients necessitates a discussion of these factors.
Specific PDE-5 Inhibitors
Sildenafil (Viagra®), vardenafil (Levitra®), and tadalafil (Cialis®) are the three oral PDE-5i's currently approved for clinical use and have become the preferred first-line ED therapy for most men due to their efficacy, safety, and ease-of-use. Published clinical trial data suggest an efficacy of ~70% for all three PDE-5i's across a wide range of causes of ED and patient subgroups.[16]
The arrival of PDE-5 inhibitors and the increased awareness of the need to evaluate potential hypogonadal states in this cohort of men has greatly improved the management of this problem, and has also increased awareness of the need by primary care physicians to evaluate both partners, individually and as an interactive unit. It is important that the primary care physician take initiative and discuss these matters with patients: patients themselves may avoid addressing issues of sexual dysfunction in a forthright matter, either asking about it at the end of a visit in passing, in connection with a separate matter, or not at all. If the physician fails to inquire, these concerns may go ignored.
Conclusion
Although the aging process is associated with many changes--both physiologic and psychosocial--in men and women, it in no way precludes continued sexual activity. Sexual relations in aging couples are an important source of gratification within the relationship. It is important for primary care physicians to discuss sexual issues in their annual visits. Be aware of the changes and the etiology and management of sexual dysfunction, and be aware of the resources available to patients.
The impact of publicity surrounding the PDE-5 inhibitors has brought sex into the public domain. It has allowed couples to seek help and begin to express their concerns. Many studies have shown the high incidence of sexual dysfunction in patients visiting their family physicians. It is essential that physicians be aware of the potential problems in couples of a sexual nature, and be prepared to allocate the time to approach the subject, and deal with the issues.[17]
Sidebar: Key Points
Sidebar: Clinical Pearls
References
- Pfeiffer E, Davis GC. Determinants of sexual behavior in middle age and old age. J Amer Geriatric Soc 1972;20:151-8.
- AARP/Modern Maturity Sexuality Study. Washington, DC: National Family Opinion Research, 1999. Online at http://assets.aarp.org/rgcenter/health/mmsexsurvey.pdf.
- Laumann EO, Nicolosi A, Glasser DB, et al. Sexual problems among women and men aged 40 to 80: prevalence and correlates identified in the Global Study of Sexual Attitudes and Behaviors. Int J Impot Res 2005;17:39-57.
- Bancroft JH. Sex and aging. New Engl J Med 2007;357:820-22.
- Marsiglio W, Donnelly D. Sexual relations in later life: a national study of married persons. J Gerontol 1991;46:S344-8.
- Masters WH, Johnson VE. Human Sexual Inadequacy. New York: Boston Little Brown, 1970.
- Masters WH, Johnson VE, Kolodny R. Heterosexuality. New York: Harper Collins, 1994.
- Laumann EO, Paik A, Rosen RD. Sexual dysfunction in the United States: prevalence and predictors. JAMA 1999;281:537-44.
- Meston CM. Aging and sexuality. West J Med 1997;167:285-90.
- Schiavi RC, Schreiner-Engel P, White D, et al. The relationship between pituitary-gonadal function and sexual behaviour in healthy aging men. Psychosom Med 1991 53:363-74.
- Zitzmann M, Faber S, Nieschlag E. Association of specific symptoms and metabolic risks with serum testosterone in older men. J Clin Endocrinol Met 2006;91:4335-43.
- Johannes CB, Araujo AB, Feldman HA, et al. Incidence of erectile dysfunction in men 40-69 years old: longitudinal results from the Massachusetts Male Aging Study. J Urol 2000;163:460-3.
- Lunenfeld B, Gooren L, Editors. Textbook of Men's Health. Parthenon Publishing Group, 2002:148-50.
- Ostatnikovà D, Celec P. Testosterone: an overview; insights into its physiology and clinical implications. Int J Endocrinol Metab 2003;2:84-96.
- Morgentaler A. Testosterone and prostate cancer: an historical perspective on a modern myth. Eur Urol 2006;50:935-9.
- Lue TF, Giuliano F, Montorsi F, et al. Summary of the recommendations on sexual dysfunctions in men. J Sex Med 2004;1:6-23.
- Nazareth I, Boynton P, King M. Problems with sexual function in people attending London general practitioners: cross sectional study. BMJ 2003;327:423.
Authors and Disclosures
Irwin W. Kuzmarov, MD, FRCSC,1 Jerald Bain, BScPhm, MD, MSc, FRCPC 2
1Department of Surgery (Urology), McGill University; Director of Professional and Hospital Services, Santa Cabrini Hospital, Montreal, QC; Past President, Canadian Society for the Study of the Aging Male
2Department of Medicine, Division of Endocrinology and Metabolism, Mount Sinai Hospital; University of Toronto, Toronto, ON; Past President, Canadian Society for the Study of the Aging Male
Disclosure: Dr. Kuzmarov has been a speaker for many companies that manufacture and/or market testosterone products, medication for erectile dysfunction, and for benign and malignant prostatic disease. Dr. Bain has given lectures at CME events sponsored by Organon Canada and Solvay Pharma,and has served on Solvay Pharma Advisory Board.
Geriatrics and Aging. 2009;12(1):53-57. © 2009 1453987 Ontario, Ltd.
testosterona,pde5,
martes, 25 de agosto de 2009
sindrome de deficiencia de testosterona:tratamiento y riesgo de cáncer
Testosterone deficiency syndrome: treatment and cancer risk.
Université Pierre & Marie Curie, 4 Place Jussieu, Paris, France. jeanpierre@raynaud.ws
Testosterone deficiency syndrome (TDS) can be linked to premature mortality and to a number of co-morbidities (such as sexual disorders, diabetes, metabolic syndrome, ...). Testosterone deficiency occurs mainly in ageing men, at a time when prostate disease (benign or malign) start to emerge. New testosterone preparations via different route of administration appeared during the last decade allowing optimized treatment to these patients. One potential complication of this treatment is the increased risk of prostate and breast cancer. Consequently, the guidelines from the agencies and the institutions, the recommendations of the scientific expert committees and the attitude of the clinicians to who, when and how to treat hypogonadal patients, is very conservative, not to say, highly restrictive. To date, as documented in many reviews on the subject, nothing has been found to support the evidence that restoring testosterone levels within normal range increases the incidence of prostate cancer. In our experience, during a long-term clinical study including 200 hypogonadal patients receiving a patch of testosterone, 50 patients ended 5 years of treatment and no prostate cancer have been reported. In fact, the incidence of prostate cancer in primary or secondary testosterone treated hypogonadal men is lower than the incidence observed in the untreated eugonadal population. However, even if the number of patients treated in well-conducted clinical trials for whom cancer of the prostate has been reported is insignificant (a very few), the observed population is still too small to raise definite conclusions. Low testosterone levels have been reported in patients undergoing radical prostatectomy and the outcomes are of worse diagnostic in this population; at a later stage, testosterone deficiency can be induced by anti hormonal manipulation of patient with a prostate cancer, leading to the symptoms of hypogonadism. The question is to know whether it is justified, in case of profound symptoms, to supplement those patients with testosterone. Some attempts have been made and the results are encouraging: so it is time to re-examine our position and to question about the definite recommendation that patients with prostate cancer should never receive testosterone supplementation therapy; this is already the situation when intermittent androgen blockade is initiated if the biological response is satisfactory. Furthermore, it has been advocated that, under a rigorous surveillance, patients cured of prostate cancer can be treated with testosterone supplementation with beneficial results.
PMID: 19429438 [PubMed - indexed for MEDLINE]
testosterona y seguridad prostatica
Testosterone and prostate safety.
Division of Urology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA 02445, USA. amorgent@bidmc.harvard.edu
For several decades it has been assumed that higher testosterone (T) leads to greater growth of benign and malignant prostate tissue, but this view has come under greater scrutiny over the last several years. Although there are as yet no large-scale, long-term controlled studies of T therapy to provide a definitive assessment of risk, numerous smaller clinical trials as well as population-based longitudinal studies consistently fail to support the historical idea that T therapy poses an increased risk of prostate cancer or exacerbation of symptoms due to benign prostatic hyperplasia. This lack of prostate risk despite increased serum T appears to be explained by data showing that exogenous T does not raise intraprostatic concentrations of T or dihydrotestosterone, suggesting a saturation model. In contrast, there is mounting evidence that low serum T is associated with greater prostate cancer risk, and more worrisome features of prostate cancer. In conclusion, the available evidence strongly suggests that T therapy is safe for the prostate. Given that the population at risk for T deficiency overlaps with the population at risk for prostate cancer, it is strongly recommended that men undergoing T therapy undergo regular monitoring for prostate cancer.
PMID: 19011298 [PubMed - indexed for MEDLINE]
2 años de tratamiento con Testosteronacon disminucion del psa en un hombre con cáncer de próstata no tratado
Two years of testosterone therapy associated with decline in prostate-specific antigen in a man with untreated prostate cancer.
Harvard Medical School, Urology, Brookline, MA, USA. amorgent@yahoo.com
INTRODUCTION: Testosterone (T) therapy has long been considered contraindicated in men with prostate cancer (PCa). However, the traditional view regarding the relationship of T to PCa has come under new scrutiny, with recent reports suggesting that PCa growth may not be greatly affected by variations in serum T within the near-physiologic range. AIM: This report details the clinical and prostate-specific antigen (PSA) response of a man with untreated PCa treated with T therapy for 2 years. METHODS: Measurements of serum PSA, total and free T concentrations were obtained at regular intervals at baseline and following initiation of T therapy. MAIN OUTCOME MEASURE: Serum PSA during T therapy. RESULTS: An 84-year-old man was seen for symptoms of hypogonadism, with serum total T within the normal range at 400 ng/dL, but with a reduced free T of 7.4 pg/mL (radioimmunoassay [RIA], reference range 10.0-55.0). PSA was 8.5 ng/mL, and 8.1 ng/mL when repeated. Prostate biopsy revealed Gleason 6 cancer in both lobes. He refused treatment for PCa, but requested T therapy, which was initiated with T gel after informed consent regarding possible cancer progression. Serum T increased to a mean value of 699 ng/dL and free T to 17.1 pg/mL. PSA declined to a nadir of 5.2 ng/mL at 10 months, increased slightly to 6.2 ng/mL at 21 months, and then declined to 3.8 ng/mL at 24 months after addition of dutasteride for voiding symptoms. No clinical PCa progression was noted. CONCLUSION: A decline in PSA was noted in a man with untreated PCa who received T therapy for 2 years. This case provides support for the notion that PCa growth may not be adversely affected by changes in serum T beyond the castrate or near-castrate range.
PMID: 19215619 [PubMed - indexed for MEDLINE
testosterona y cáncer de próstata,model saturacion
Shifting the paradigm of testosterone and prostate cancer: the saturation model and the limits of androgen-dependent growth.
Division of Urology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts, USA. amorgent@yahoo.com
CONTEXT: The traditional belief that prostate cancer (PCa) growth is dependent on serum testosterone (T) level has been challenged by recent negative studies in noncastrated men. OBJECTIVE: To provide an improved framework for understanding the relationship of PCa to serum T level that is consistent with current evidence and is based on established biochemical principles of androgen action within the prostate. EVIDENCE ACQUISITION: A literature search was performed of publications dating from 1941 to 2008 that addressed experimental and clinical effects of androgens on prostate growth. Review of studies investigating the prostatic effects of manipulation of androgen concentrations in human and animal studies, and in PCa cell lines. EVIDENCE SYNTHESIS: Prostate growth is exquisitely sensitive to variations in androgen concentrations at very low concentrations, but becomes insensitive to changes in androgen concentrations at higher levels. This pattern is consistent with the observation that androgens exert their prostatic effects primarily via binding to the androgen receptor (AR), and that maximal androgen-AR binding is achieved at serum T concentrations well below the physiologic range. A Saturation Model is proposed that accounts for the seemingly contradictory results in human PCa studies. Changes in serum T concentrations below the point of maximal androgen-AR binding will elicit substantial changes in PCa growth, as seen with castration, or with T administration to previously castrated men. In contrast, once maximal androgen-AR binding is reached the presence of additional androgen produces little further effect. CONCLUSIONS: The evidence clearly indicates that there is a limit to the ability of androgens to stimulate PCa growth. A Saturation Model based on androgen-AR binding provides a satisfactory conceptual framework to account for the dramatic effects seen with castration as well as the minor impact of T administration in noncastrated men.
PMID: 18838208 [PubMed - in process]
terapia con testosterona en hombres con cáncer de próstata,consideraciones scientificas y eticas
Testosterone therapy in men with prostate cancer: scientific and ethical considerations.
Men's Health Boston and the Department of Urology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts, USA.
PURPOSE: Pertinent literature regarding the potential use of testosterone therapy in men with prostate cancer is reviewed and synthesized. MATERIALS AND METHODS: A literature search was performed of English language publications on testosterone administration in men with a known history of prostate cancer and investigation of the effects of androgen concentrations on prostate parameters, especially prostate specific antigen. RESULTS: The prohibition against the use of testosterone therapy in men with a history of prostate cancer is based on a model that assumes the androgen sensitivity of prostate cancer extends throughout the range of testosterone concentrations. Although it is clear that prostate cancer is exquisitely sensitive to changes in serum testosterone at low concentrations, there is considerable evidence that prostate cancer growth becomes androgen indifferent at higher concentrations. The most likely mechanism for this loss of androgen sensitivity at higher testosterone concentrations is the finite capacity of the androgen receptor to bind androgen. This saturation model explains why serum testosterone appears unrelated to prostate cancer risk in the general population and why testosterone administration in men with metastatic prostate cancer causes rapid progression in castrated but not hormonally intact men. Worrisome features of prostate cancer such as high Gleason score, extracapsular disease and biochemical recurrence after surgery have been reported in association with low but not high testosterone. In 6 uncontrolled studies results of testosterone therapy have been reported after radical prostatectomy, external beam radiation therapy or brachytherapy. In a total of 111 men 2 (1.8%) biochemical recurrences were observed. Anecdotal evidence suggests that testosterone therapy does not necessarily cause increased prostate specific antigen even in men with untreated prostate cancer. CONCLUSIONS: Although no controlled studies have been performed to date to document the safety of testosterone therapy in men with prostate cancer, the limited available evidence suggests that such treatment may not pose an undue risk of prostate cancer recurrence or progression.
PMID: 19150547 [PubMed - indexed for MEDLINE]
El papel de la testosterona en el sindrome metabolico,revision
: J Steroid Biochem Mol Biol. 2009 Mar;114(1-2):40-3.Links
The role of testosterone in the metabolic syndrome: a review.
Men's Healthcare, Scientific Affairs Bayer Schering Pharma AG, Berlin, Germany. Farid.Saad@bayerhealthcare.com
Over the last three decades it has become apparent that testosterone plays a significant role in the maintenance of bone and muscle mass, in erythropoiesis, and in mental functions. But testosterone is also a key player in glucose homeostasis and lipid metabolism. The metabolic syndrome is a clustering of risk factors predisposing to late onset diabetes mellitus, atherosclerosis and cardiovascular morbidity and mortality. The main components of the syndrome are visceral obesity, glucose intolerance, raised blood pressure and dyslipidaemia (elevated triglycerides, low levels of high-density lipoprotein cholesterol),and a pro-inflammatory and thrombogenic state. Cross-sectional epidemiological studies have reported a direct correlation between plasma testosterone and insulin sensitivity, and low testosterone levels are associated with an increased risk of type 2 diabetes mellitus, dramatically illustrated by androgen deprivation in men with prostate carcinoma. Lower total testosterone and sex hormone-binding globulin(SHBG) predict a higher incidence of the metabolic syndrome. There is now evidence to argue that hypotestosteronaemia should be an element in the definition of the metabolic syndrome. Administration of testosterone to hypogonadal men reverses the unfavorable risk profile for the development of diabetes and atherosclerosis. Testosterone should be regarded as a pivotal hormone for men's health.
PMID: 19444934 [PubMed - indexed for MEDLINE]
Suscribirse a:
Entradas (Atom)